What factors could explain Covid-19's deadly impact in Catalonia?
Age, population density, health care, or preparedness hold the key to understanding what went wrong

Catalonia has been notoriously hard hit by the coronavirus pandemic, both in comparison to most of the rest of Spain, except for Madrid, as well as other parts of Europe and the world.
And yet, it is still too early to come to final conclusions on why this has been the case here and perhaps not elsewhere as more time will be needed both to gather further information and for data standardization.
With this in mind, we have come up with a list of potential factors - which in no case should be considered in isolation, but rather in conjunction with others - that could possibly help to explain this phenomenon in Catalonia.
Age
One thing that has become clear since the beginning of the outbreak is that the older a Covid-19 patient is, the greater the likelihood of there being a negative outcome, with a similar tendency found among those with underlying health conditions.
Catalonia, as well as the rest of Spain, has both low birth rates and a higher than average initial maternal age, with an aging index - population over 65 per 100 inhabitants under 15 - of 121.6 (Idescat, 2019). There has been some speculation that this could explain why some places have been more affected than others - for example, Iran has over 100,000 confirmed cases, but its young population has experienced fewer deaths than many European countries.
Yet age alone isn't enough: Japan, relatively far closer to Wuhan than Iran or Europe, has had just over 550 coronavirus-related fatalities, and other parts of Europe have higher average ages than Catalonia, including Germany, with fewer deaths.
That said, age groups first affected by the virus do vary from country to country. "In Spain, it seems it has hit a lot in the care homes. Obviously, with so many old people there, the mortality rates are much higher, whereas in Germany, the first batch of people infected were young people," explains Catalan medical researcher Salvador Macip, adding that many had recently gone skiing in Italy before returning to their home country.
Population density
The higher the population density, the higher the chances are of transmitting the virus to a greater number of people in highly transited spaces, such as an overly crowded public transport system or supermarkets, for example.
Although Catalonia’s average population density is only 239,0 hab./km2, in urban areas that number is much higher. These are precisely the places that - with some explainable exceptions, like in Anoia due to the Igualada cluster - have been more affected than its less populous areas.
It is also worth noting that Barcelona and its surroundings are much more densely populated than plenty of other large metropolitan areas - 16,149.6 inhabitants per km2 (Idescat, 2019) compared to London’s 5,666.7 (ONS, 2018 / 1,572 km²) and New York’s 10,715.42 (US Census Bureau, 2018 / 783.8 km²). And other densely populated cities, like Paris, only provide data on PCR positives, while the Catalan capital’s confirmed cases also include other kinds of tests: 7,911 PCR positives (May 4) versus 17,008 PCR and other positives (May 7), respectively.
Stockholm, on the other hand, has under a million residents in the city proper and a population density of around 5,181.2 (SCB, 2019 / 188 km²). In Sweden, the European exception where lockdown was not implemented, there are far fewer deaths than in Catalonia or Spain, but its fatalities surpass neighboring Denmark and Norway combined, where confinement rules were in order.
But there are other metropoles with similar or higher densities but fewer cases. Density alone cannot explain the virus' prevalence - it must be considered alongside an array of other possible factors, including the movement of people - especially between areas with notable outbreaks, such as northern Italy, where Catalonia's first documented cases originated - and more.
Strength of the public health system
The 2008 financial crisis and subsequent austerity measures greatly weakened Catalonia's public health system, reinforcing the trend towards a reduction of beds and doctors. "What they did with the cuts is basically scale down to as much as the system can take, which is fine if the system works it can survive, but it cannot deal with a crisis, which is what we see now," Macip argues.
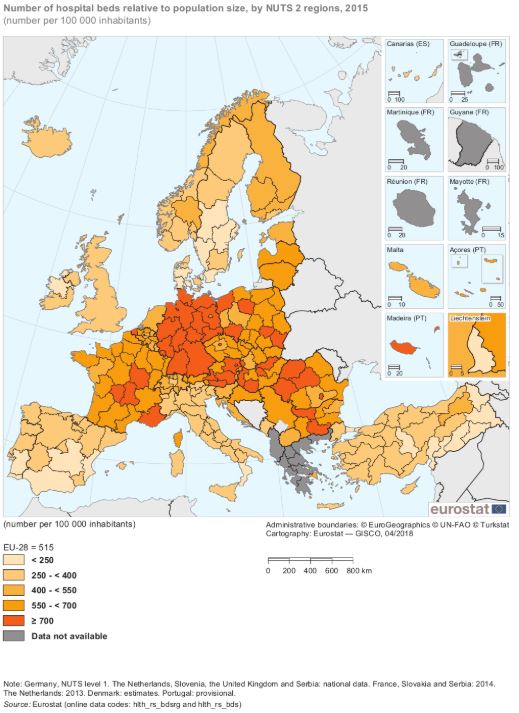
As can be seen in the 2015 Eurostat map above, Catalonia has fewer hospital beds per capita than France, Germany or the Netherlands, but has a similar number to those found in parts of also hard-hit Italy and the UK. And in other countries with austerity-weakened public health systems, swifter measures were imposed when there were still even fewer confirmed Covid-19 cases and deaths than in Catalonia when it was forced under lockdown.
"It could be that some countries have been more severe in terms of applying things like lockdown," says Macip. "We've seen countries like Greece, for instance, that seems to have done a pretty good job at keeping people inside their homes," which has translated into Covid-19 figures remaining far lower than in western European nations: as of May 7, some 2,663 diagnoses and 147 deaths.
Recentralization v. continued devolution
Arguments - often accused of being tinged with the underlying tensions between the Catalan and Spanish governments, and sometimes rightfully so - have been heard both in favor and against the centralization of authority to deal with coronavirus crisis.
In Spain, and under normal circumstances, health is controlled by the regions but authority over this domain was exceptionally recentralized with the state of alarm. As Macip sees it, "the Spanish government was perhaps not ready or prepared to have centralized control because, by default, all the power in terms of health is already devolved into the regions."
And like others, he also believes that federal Germany has handled the crisis better: "It seems to show that it works better if you keep a center of control but you give the power to the different regions and let them manage their cases in a rational way based on their own reality."
Whether systems of devolved power work better than centralized ones is debatable, as is the argument that perhaps existing health structures should not have been disrupted in favor of new lines of command. But in any case, and regardless of who may have the "right" answer, the continual discord between Spanish and Catalan authorities with regards to crisis management - from the timing and the severity of lockdown to the unit of reference for easing it, which was eventually agreed on - cannot have helped instill confidence among the public.
Preparation and management
Epidemiologists are tasked with the monumental challenge of trying to both convince politicians and the public of the existence of risk before evidence of it is visible to the layperson's eye as well as of persuading society to carry on with a wildly different course of action - gravely disrupting social practices and the economy - before the threat actually arrives in full force. And sometimes, as was perhaps the case here with Oriol Mitjà's warnings, they are not heeded.
5)𝗛𝗮𝘆 𝗾𝘂𝗲 𝗽𝗮𝗿𝗮𝗿𝗹𝗼 𝘁𝗼𝗱𝗼 𝟮 𝘀𝗲𝗺𝗮𝗻𝗮𝘀. El confinamiento debe ser total (a excepción de trabajadores en servicios básicos y alimentación). Imágenes de los transportes públicos llenos muestran que nuestros responsables siguen sin entender la gravedad del asunto
— Oriol Mitjà (@oriolmitja) March 16, 2020
In other parts of the world, however, action was taken much more swiftly than in Catalonia - where President Quim Torra was still blaming the cancellation of the Mobile World Congress on "an epidemic of fear" - or in Spain, where life in early March, for the most part, went on as usual despite proximity to the outbreak that was already raging in northern Italy.
One hypothesis that could explain the rapid response of other countries is familiarity with public health crises. In South Korea, home to the biggest MERS outbreak outside the Middle East in 2015, the use of face masks was embraced early on and authorities reacted quickly by carrying out mass Covid-19 testing and contact tracing. And perhaps for other Asian countries, the 2002-2003 SARS epidemic still remained a vivid memory.
Understanding the data
Attempting to make accurate comparisons between regions and countries is made even more difficult by variations in data collection methodology, reporting delays, as well as differences in the overall number of tests in relation to the population as well as the kind of diagnostic test used.
In Catalonia, the confirmed Covid-19 cases that are announced by the Health Department every night include both PCR and rapid test positives, which are known for being inaccurate at times, while the figures the Spanish Ministry of Health proclaims daily are of PCR positives, with some information on serological tests included in its press releases. Yet, we don't have to go too far to see Spain is not the only country to do so - French government statistics, for example, focus mainly on PCR results as well, though their information is not clearly differentiated outside of major cities and laboratories.
Besides this, the official deaths count in Spain, as in most other parts of the world, includes only people who had been diagnosed. But not everywhere are a proportionate number of tests carried out among residents, meaning that many cases and deaths may go unaccounted for. Catalonia, with a population of 7.72 million (Idescat, 2019), had carried out some 302,000 PCR diagnostic tests - some on the same person more than once - by May 4 according to Catalan health minister Alba Vergés.
The Our World in Data map below can help provide us with an idea of how many tests have been carried out in relative to the total population - suggesting that Covid-19 cases and deaths could be undercounted in many places - although again, the data cannot be fully trusted either as not enough information has been gathered and standardized yet.
Other places, like Belgium - one of the few European countries with a higher death rate per million inhabitants than Spain - includes both confirmed and suspected coronavirus-related fatalities in its death count, which would in part explain why its numbers are much higher.
This could also lead one to believe that considering excess mortality may be useful when trying to gauge the scope of the pandemic. Data compiled by Euromomo, a European mortality monitoring group, shows that other parts of Europe, like the United Kingdom, Sweden, Italy, or The Netherlands have higher excess mortality rates than Spain as of Week 17, possibly implying higher Covid-19 numbers than those reported.
Readers may also remember one of the clashes between Catalan and Spanish authorities a few weeks back was precisely over the official toll - first because it only included deaths at medical centers, leaving out the sizable number of elderly dying at care homes and elsewhere, and then because it did not account for the much higher numbers reported by funeral homes.
The Catalan health department now releases daily numbers of confirmed and suspected Covid-19 deaths at medical centers as well as those reported by funeral homes, which do not fit seamlessly into the Spanish ministry of health's daily press releases, although the data is likely provided directly to the central government in following with its preferred methodology.
If anything, these methodological discrepancies across borders indicate that currently available data sets can only provide us with a partial idea of the havoc the pandemic has been wreaking. For now, it seems we can only hope to make informed guesses as to what exactly went wrong.